Viral Sign is superior to the best thermography result published by Singapore-based researchers during the SARS-2003 outbreak.
SARS-2003
Accuracy
93%
Sensitivity
85%
Viral Sign
Accuracy
96%
Sensitivity
95%
False negatives: The great challenge of this pandemic.
Less than 30% of people have a temperature higher than 37.8ºC in the first 5 days after becoming infected with COVID-19. As a result, there is great risk for a large number of false negatives.
Symptomatic screening with a single point body temperature permits individuals who are “false negatives”, infected but without fever, to enter factories, healthcare facilities, schools, government buildings, and other centers where people gather.
The virus thrives on false negatives.
Liu T, Zhang J, Yang Y, Zhang L, Ma H, Li Z, et al. The potential role of IL-6 in monitoring coronavirus disease 2019. medRxiv. 2020.
How does Viral Sign differ from point (thermometer) and mass temperature (thermal camera) assessment?

Both point thermometers and thermal cameras are based on a single maximum temperature point.
This greatly diminishes the efficacy of these screening methods due to distance, temperature, and ambient humidity. The appropriateness of the target, or area where the device is pointed, and the steadiness of the device can alter the temperature result. And, or course, the virus may be present, but not symptomatic (with fever).
Point clinical thermometer temperature assessment evaluates a single point on the forehead, ear or wrist.The weaknesses of point thermometer measurement include:
- Great variability in readings and lower accuracy,
- Exposes the operator to risk of infection from the individuals the operator encounters for screening,
- Exposes those being screened to a person (the operator) who may be infected.

Thermal cameras cannot identify the presence of virus prior to the onset of fever.
Thermal cameras cannot identify the presence of virus prior to the onset of fever.
The measurement of only elevated body temperature, based on fixed values such as 37.5 degrees Celsius or 99.6 degrees Fahrenheit, is not enough to track cases of people infected with COVID-19.
Despite receiving an image representing several temperature points, thermal cameras rely only on a single point of maximum temperature. This is similar in many respects to the use of point temperature thermometers.
In addition, thermal cameras do not limit the analysis of temperature to the maximum temperature point of human skin. The thermal camera can randomly retrieve temperature measurements outside the human body.
The eyes are a region that can get more or less moist due to tears. Tearing in the eyes does not correlate with fever.
Vascular diseases or lesions in this region of the face can hinder the analysis also based on a single point.
The maximum temperature of the body surface is not always the most effective way to know if the person is infected by the new coronavirus (COVID19).
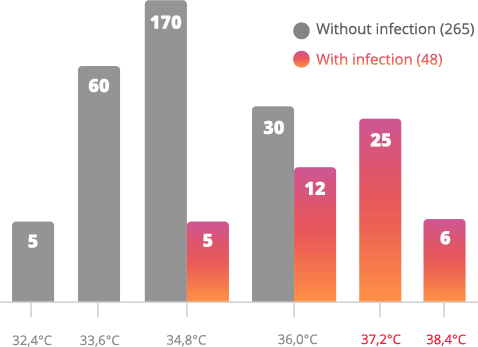
Number of people infected with eye temperature below 37.2 C (no fever).
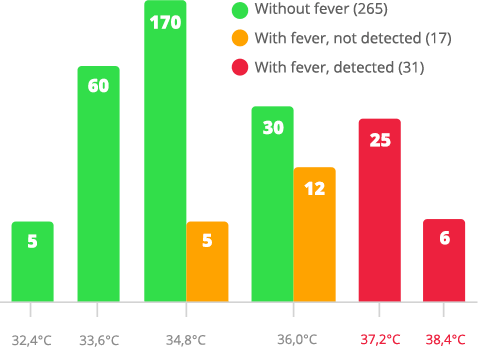
Body temperature measurement of 313 people.
Conventional Thermography
35% of people with fever had eye temperature below 37.2C.
Identified only 31 people with fever
The problem with traditional thermography is that people can be contaminated even without fever.
Viral Sign
All people (with and without fever) were screened correctly by ViralSign™, regardless of eye temperature.
Correct indentification of the 48 people infected